Last Updated on: 13th February 2024, 05:47 pm
Pericarditis, an inflammation of the pericardium often leading to fluid accumulation in the pericardial space, is a disorder that can stem from various causes, including infections, myocardial infarctions, traumas, neoplasms, and metabolic disorders. However, it often presents without an identifiable cause, hence being termed idiopathic.
Patients suffering from pericarditis often complain of chest pain or a feeling of constriction, symptoms that may worsen with deep breaths. In more severe cases, such as cardiac tamponade or constrictive pericarditis, cardiac function can be significantly compromised.
Diagnosis relies on clinical symptoms, signs such as pericardial friction rub, ECG alterations, and the presence of pericardial fluid detectable through radiography or echocardiogram. Investigating the underlying cause requires further tests, while treatment varies depending on the etiology, including the use of analgesics, anti-inflammatory drugs, colchicine, and, in rare cases, surgical interventions.
What is Pericardium and it’s Types
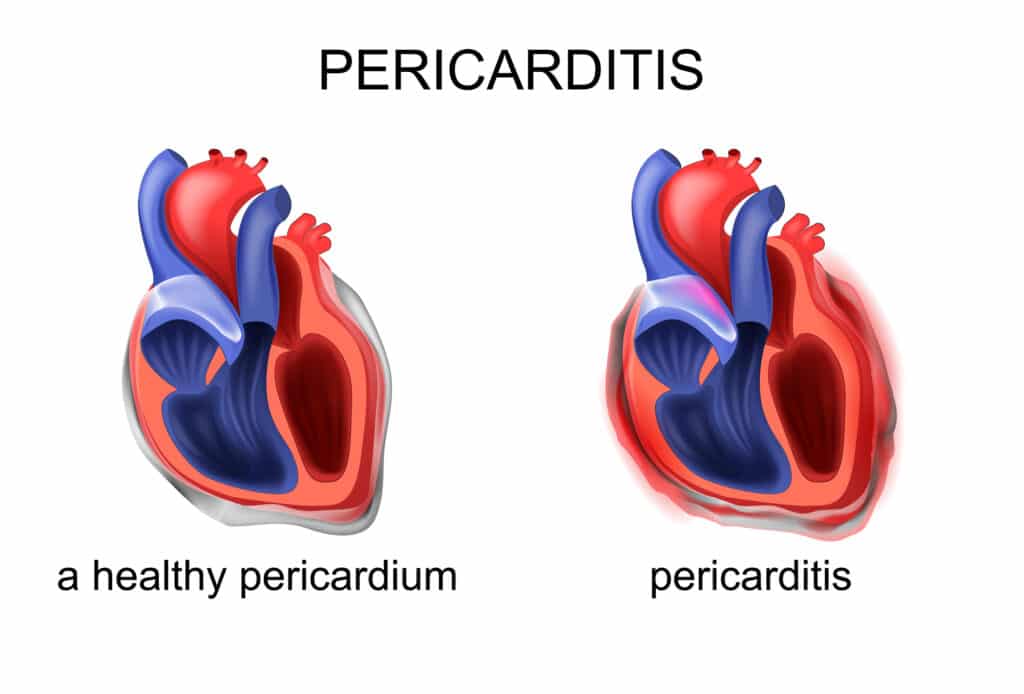
The pericardium consists of two layers: the visceral layer, a thin layer of mesothelial cells adhering to the myocardium, and the parietal layer, a fibrous sheet that, together with the visceral layer, encloses the heart. This structure contains a small amount of fluid, which serves to limit the distension of the cardiac cavities and optimize cardiac efficiency.

Pericarditis can manifest in acute, subacute, or chronic forms, with acute pericarditis characterized by rapid development of inflammation and potential fluid accumulation (pericardial effusion). This condition can progress to subacute or chronic pericarditis, with chronic pericarditis defined by the persistence of inflammation beyond six months.
Pericardial effusion, the accumulation of fluid in the pericardial space, can vary in composition and, in extreme cases, lead to cardiac tamponade, a potentially lethal condition in which abundant effusion obstructs cardiac filling.
Conversely, constrictive pericarditis is characterized by marked thickening of the pericardium, reducing ventricular filling capacity, negatively impacting cardiac output, and potentially leading to systemic venous congestion conditions.
Causes of Pericarditis
Acute pericarditis is a clinical entity with a wide variety of causes, ranging from infections to autoimmune diseases, traumas, and metabolic conditions such as uremia. This etiological diversity renders the disorder a true pathogenetic mosaic, with direct implications for patient treatment and prognosis.
The Infectious and Autoimmune Puzzle
Most cases of acute pericarditis are presumed to be of viral origin, although often the cause remains idiopathic, meaning unknown or unidentified. Purulent bacterial pericarditis, although less common, represents a medical emergency given the potential evolution towards severe complications. Other infectious causes include fungi, parasites, and, in endemic areas, tuberculosis.
From Infarction to Direct Damage: Unexpected Pathways
Acute myocardial infarction can precipitate pericarditis in 10-15% of cases, underscoring how major cardiac events can have repercussions on the pericardial sac. Post-infarction syndrome (Dressler’s syndrome) and post-pericardiotomy syndrome further highlight the link between direct cardiac damage and inflammatory pericardial response.
Chronic Pericarditis: Beyond Acuity
No less important is chronic pericarditis, which may present with or without a preceding acute episode. The presence of chronic pericardial effusion, sometimes hemorrhagic in nature, suggests possible neoplastic etiologies, including lung or breast carcinoma. Metabolic conditions such as hypothyroidism can also cause cholesterol pericarditis, rare but significant for its association with myxedema.
Symptoms
The clinical presentation of pericarditis varies greatly depending on the stage of the disease, from the acute phase characterized by chest pain, fever, and pericardial friction rub, to manifestations of constriction or cardiac tamponade in more advanced stages. Constrictive pericarditis, in particular, poses unique diagnostic and therapeutic challenges, given its ability to mimic other systemic venous congestion conditions.
Diagnosis
Diagnosing pericarditis is a journey through clinical signs, advanced technologies, and laboratory investigations, aiming to identify not only the presence of pathology but also its underlying cause.
The First Step: ECG and Chest X-ray
The diagnostic process begins by examining the electrocardiogram (ECG) and performing a chest X-ray. The ECG helps identify anomalies such as ST and PR segment changes, indicating cardiac issues. On the other hand, the chest X-ray can show whether the heart is enlarged, a sign that may indicate the presence of fluid in the pericardium, the sac surrounding the heart.
Echocardiography: A Window to the Heart
Echocardiography is crucial as it allows visualization of fluid in the pericardium, detection of problems in how the heart fills indicating cardiac tamponade, and identification of cardiac muscle involvement. This non-invasive method provides a clear, real-time view of the heart at work, offering important insights into the condition of the pericardium.
From Aspiration to Pericardial Biopsy
To understand the exact cause of pericarditis, it may be necessary to aspirate fluid from the pericardium or perform a pericardial biopsy. These tests offer concrete samples to analyze, helping to discover whether pericarditis is due to infections, inflammations, or tumors, and allowing the selection of the most appropriate treatment.
The Challenge of Acute Pericarditis
In the case of acute pericarditis, diagnosis is based on three main elements: chest pain typical of this condition, the sound of pericardial friction rub heard with a stethoscope, and abnormalities detectable with an electrocardiogram (ECG), which can be confirmed by the presence of fluid in the pericardium. ECG changes can manifest in four successive phases, each indicative of different degrees of pericardial inflammation.
The finding of pericardial fluid increases suspicion towards this diagnosis, often confirmed by echocardiography. The latter can show how much fluid has accumulated and how this is affecting heart function. Other tests, such as chest X-ray and ECG, can provide additional information, such as showing an enlarged heart or weaker than normal electrical signals, characteristic of low QRS voltages.
Constrictive Pericarditis: A Diagnostic Enigma
To diagnose constrictive pericarditis, an approach involving various specialists and diagnostic techniques is necessary, including electrocardiogram (ECG), chest X-ray, Doppler echocardiography, cardiac catheterization, and advanced imaging techniques such as computed tomography (CT) or magnetic resonance imaging (MRI).
These methods allow differentiation of constrictive pericarditis from other conditions presenting similar symptoms, such as restrictive cardiomyopathy, providing detailed information on the heart and pericardium.
Identifying the underlying cause of pericarditis is crucial to direct treatment. Evaluation can range from analysis of pericardial fluid and biopsies to serological and immunological tests, depending on clinical circumstances and etiological suspicions. Pericardiocentesis and surgical drainage offer both diagnosis and therapy in selected cases.
Treatment and Management: Personalized and Targeted
The treatment of pericarditis depends on its cause and severity. Nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine may be used to control inflammation and prevent new episodes. In more serious cases, more direct interventions such as pericardiocentesis or pericardiectomy may be necessary. Additionally, if cardiac tamponade occurs, immediate intervention is crucial to avoid serious health risks.
Dealing with pericarditis requires a tailored treatment plan, taking into account how severe the condition is, its causes, and any complications. The care plan varies from using less invasive therapies to surgical interventions, with the main goal being to alleviate pain, reduce inflammation, and cure the underlying cause.
For acute pericarditis, the initial approach involves nonsteroidal anti-inflammatory drugs and colchicine, which are effective in reducing the likelihood of recurrence. It is important to adjust the dosage of these drugs based on the specific situation of the patient and their response to treatment.
When to Intervene: Pericardiocentesis and Corticosteroids
In cases of cardiac tamponade or when significant pericardial effusions are present, pericardiocentesis is a crucial treatment that allows the removal of fluid from the pericardium, relieving pressure on the heart. The use of ultrasound increases the safety and effectiveness of this procedure.
For more stubborn cases or when there are specific reasons, such as autoimmune or uremic pericarditis, corticosteroids may be considered, but with caution due to possible side effects, such as increased viral replication and the risk of recurrences when the dosage is tapered.
Advanced Treatment Options
More targeted treatments may be adopted in specific situations, such as injecting drugs directly into the pericardium to reduce inflammation while minimizing side effects on the rest of the body. Pericardial resection, although rare, may become necessary in cases of constrictive pericarditis that do not respond to conventional therapy.
Addressing the Root Cause
It is essential to identify and treat the primary cause of pericarditis, which can range from managing underlying conditions such as cancer with specific therapies. The treatment approach must be comprehensive and personalized, considering all possible causes of the disease and adapting the therapeutic strategy accordingly.
Practical Considerations
Hospitalization may be necessary for high-risk patients or those requiring monitoring for the development of cardiac tamponade. Careful follow-up is crucial for all patients, regardless of the treatment setting.
Additionally, it is essential to assess the use of any drugs that may contribute to the etiology of pericarditis, considering discontinuation of such agents if indicated.
You can also read the Nipah Virus: Origin, Symptoms, Diagnosis, Treatment, Outbreak, and Cases.
Managing pericarditis requires careful clinical evaluation, accurate therapeutic selection, and customization of treatment based on the individual needs of the patient. Through the targeted use of pharmacological therapies, procedural interventions, and treatment of underlying causes, symptom control and prevention of recurrences can be achieved, guiding patients toward optimal recovery.

Researcher, Blogger, Content Writer, Online Marketing Expert, Aptitude Test & Admissions Expert, Career Counselor.
PEC REGISTERED. ENGINEER. (ARMY MED. COLLEGE)
CEO / Founder (The Educationist Hub)